Earlier Specialized Physician Intervention Lowers Costs, Readmissions and Length of Stay
Overview
In an innovative approach to wound care management, two Midwest hospitals partnered with Healogics to create a program that emphasized earlier intervention and a higher level of wound care integration throughout the care continuum. An initial pilot project demonstrated considerable successes in the reduction of care costs, readmissions and length of stay for hospital inpatients patients with chronic wounds – a group that typically ranks highest in these three areas.
This hospital’s approach and experience suggests steps that other hospitals can take to improve wound center outcomes by enhancing existing strengths in wound care, all with minimal impact on established workflows.
Solving Challenges
When two Midwestern hospitals partnered with Healogics to establish a new wound center, it was an opportunity to address issues common to chronic wound care. While hospitals typically do a very good job of dressing wounds, wound centers do not typically engage with patients beginning with admission, and wound care management does not typically follow the patient post-discharge. This suggests opportunities for improvement. Because patients with chronic wounds are often among the sickest patients due to underlying conditions such as diabetes, they are also the most vulnerable to longer length of stay, and more prone to readmission. In establishing
this particular wound center, the hospital agreed to try an elevated form of wound care case management that integrated wound care throughout each episode of care, starting with admission and continuing post-discharge.
After building the wound center, Healogics and hospital leadership created a plan for wound management that emphasized early interventions, coordinated collaboration with other physicians and nursing staff and continuing post-acute wound care. There were two overriding requirements for the plan:
- There were to be as few modifications as possible to established hospital workflows.
- Care teams were to be educated in the importance of the approach, not as a replacement to existing skillsets, but as an enhancement to improve outcomes for high-cost patients.
With support from the hospital’s CMO and medical leadership, the Healogics physician worked with care team leaders to develop a methodology for inpatient wound care. Key elements included protocols to determine which wounds need consultation, when consultations were to occur, and specifying those that require intervention at admission. Discharge protocols identified which patients were at the greatest risk of readmission if sent home and should instead move to skilled nursing facilities with standards of quality comparable to the wound center’s standards, ensuring greater continuity of care.
To measure the impact of this approach, the hospital deployed the new system on a control group and measured the control group’s outcomes along with outcomes for patients following standard care protocols. For the control group, average days to first consultation were 0-2 days, versus a more typical 3-8 days.
Results
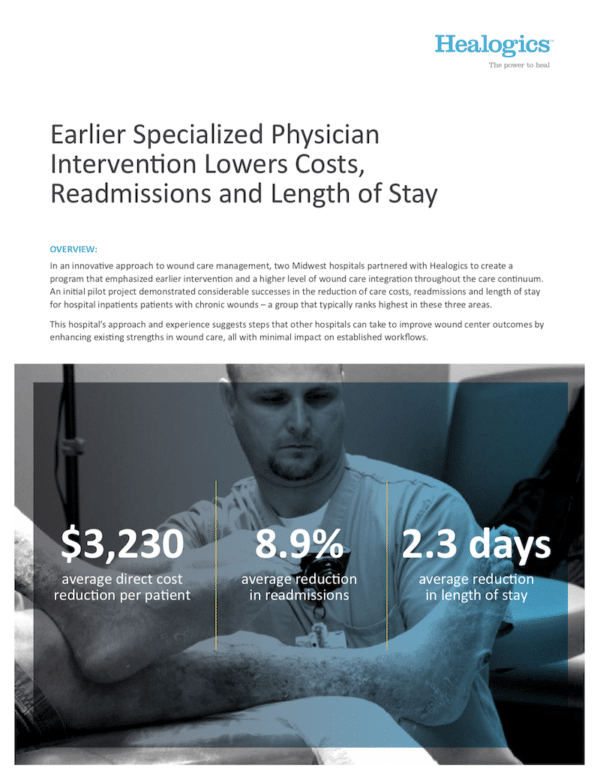
This health system’s experience demonstrates the positive impact of a dedicated and focused wound care specialty physician and integrated wound care with the care team throughout entire episodes of care. Earlier interventions enabled a focus on key diagnoses and therapies sooner and wound patients received skilled bedside wound care that continued through post-discharge. Improvements for the
control group included:
- Reduction of average daily medical costs from $10,670 to $7,440 – an average medical cost savings of $3,230 per day per patient.
- Readmission rate reduction from 23.4% to 14.5%, for an overall 8.9% improvement in readmissions for patients with chronic wounds.
- Average LOS reduction from 9.41 days to 7.11 days, meaning these patients were discharged on average 2.3 days sooner than those not in the control group.
These improvements brought patients with chronic wounds more in-line with the metrics of non-wound patients during the same period.