Curative Versus Palliative Wound Care
May 2, 2023What Is Palliative Wound Care?
According to the Center to Advance Palliative Care, palliative care is “specialized medical care for people living with a serious illness. This type of care is focused on providing relief from the symptoms and stress of the illness. The goal is to improve quality of life for both the patient and the family. … Palliative care sees the person beyond the disease. It is a fundamental shift in healthcare delivery.”
Although it is a common misconception even among healthcare providers, palliative care is not hospice care. Hospice care is intended for people who are near the end of life. It does not include intentions meant to cure disease or prolong life. In contrast, palliative care is “appropriate at any age and at any stage in a serious illness, and it can be provided along with curative treatment.”
Palliative wound care has four main objectives:
- Drainage
- Odor control
- Infection prevention
- Pain management
Curative Versus Palliative Wound Care
Most patients who enroll in a wound program have a primary goal to heal the wound. Palliation can and should be included as part of the curative plan to address pain, drainage, and odor.
Yet even with the best wound care available, not all wounds achieve closure. Perhaps a patient has received multiple evidence-based interventions that were unsuccessful, such as antibiotics, debridement, hyperbaric oxygen therapy, bone debridement, and the most advanced wound dressings available. Or perhaps the intervention that could help poses greater risk to the patient than the wound does. For example, surgery to improve tissue perfusion may not be possible in some people or may be too risky.
At this point, the patient, family, and healthcare team can use shared decision-making to shift the focus regarding the goals of care. Palliation, symptom relief, and quality of life become the primary objectives, and curative goals become secondary.
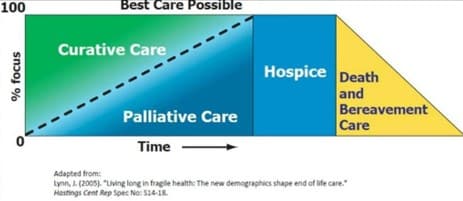
This concept is illustrated in the diagram above. Curative care is the primary initial focus for most cases; however, palliative measures are included. Over time, in a small number of patients, the goals of care can change, with a decreased emphasis on curing and an increasing focus on palliation. In patients near end of life, hospice becomes the focus.
The need for palliative wound care affects a wide variety of patients, including:
- Younger people who’ve experienced traumatic injuries. These patients often need palliative measures, including pain management, rehabilitative needs, and social and family support needs.
- Middle-aged, active individuals who have comorbid conditions that affect wound-healing options
- Patients with cancer
- People at the end of life
Healthcare providers in many settings—from trauma centers, emergency departments, geriatric practices, hospices, long-term care facilities, skilled nursing facilities, and more—must be thoughtful about realistic expectations and goals of care. There may come a time when the best care is palliative care.
A Patient-Centered Approach
Palliative care can be a sharp contrast to our expectations. Our health system and our culture have conditioned both patients and healthcare professionals to prioritize and expect cure. Similarly, wound care as a medical specialty is designed—even expected—to achieve wound closure for every patient.
But patient-centered care requires that we reconsider that mindset with a thoughtful, individualized approach to each person’s needs and priorities. The decision to shift to palliative wound care should take the following factors into consideration:
- Challenges inherent with following through with available treatments (e.g., time and energy booking and attending appointments, missed work, recovery time, side effects)
- Comparative costs of care
- Life expectancy, considering overall health and all comorbid conditions
- Quality of life, such as ability to participate in activities and self-consciousness about a wound (e.g., odor)
- Realistic expectations whether curative treatments will help
Often, patients who receive palliative care are some of the most satisfied and grateful patients. Many say they wish they had chosen palliative options much earlier. Not only can palliative wound care be life-changing for patients, but it also can be very rewarding for healthcare providers. Palliative wound care can be an opportunity to make a meaningful difference in a patient’s daily activities, quality of life, and mental well-being.
Options for Wounds in the Palliative Setting
It’s important to note that palliative wound care is not equivalent to no wound care. When you move to a palliative care model, you are not abandoning hope or withholding treatment. Rather, you are thoughtfully making a paradigm shift that reprioritizes the goals of care.
Many healthcare providers may be surprised that there are still interventions that can make a significant positive difference in the lives of patients with non-healing wounds. For example:
- Antiseptics that are not appropriate for healing tissue but can control bacterial load
- Amputation
- Dressings specifically designed to absorb odor
- Dressings that contain silicone to facilitate drainage or are suffused with topical pain solutions
- Negative pressure wound therapy (vacuum-assisted) to assist with drainage and infection control
- Surgical debridement to reduce but not eliminate infected tissue, with goals such as odor control
The idea is to be thoughtful about what truly is best for the patient, perhaps even the most time efficient and cost effective. This may not always be what it seems. For example, advanced modalities such as negative pressure wound therapy can reduce costs and time commitments for some patients because it reduces the needs for nursing care, dressing changes, and medications for pain.
Wound Care at the End of Life
Patients with limited life expectancy and non-healing wounds can benefit from palliative treatment to improve quality of life. Wound care specialists can make a very significant impact in hospice patients with pressure, venous, arterial, diabetic, or neuropathic ulcers.
Wound care interventions can help these patients rest more comfortably, as well as reduce odors to facilitate family visits. Palliative wound care can help people spend the end of their lives more peacefully and respectfully in line with their wishes.

By William J. Ennis
William J. Ennis, DO, MBA, MMM, CPE, is chief medical officer of Healogics, the nation’s leading provider of advanced wound care. He also serves as the Catherine and Francis Burzik Professor of Wound Healing and Tissue Repair and chief of the Section of Wound Healing at the University of Illinois at Chicago’s Division of Vascular Surgery.
