Peripheral Artery Disease (PAD)
Peripheral Artery Disease (PAD) is a serious circulatory condition in which fatty plaque (atherosclerosis) builds up in peripheral arteries—especially those supplying the legs—narrowing or blocking blood flow. It affects nearly 10 million Americans, particularly people over age 65, and can lead to poor wound healing, infections, and an increased risk of lower-limb amputation if left untreated. Understanding PAD early gives you a better chance to manage symptoms, prevent complications, and protect your mobility.
Understanding PAD and Its Causes
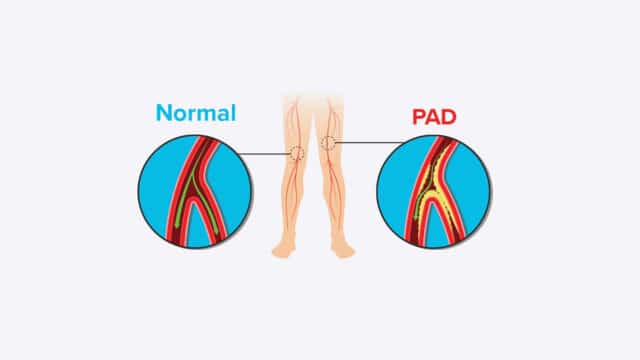
PAD develops when plaque and fatty deposits (atherosclerosis) accumulate inside the peripheral arteries, reducing blood flow to the lower extremities. This process damages tissue by limiting oxygen and nutrient delivery.
Some contributors are non-modifiable—like age and family history—while others are lifestyle-related and therefore addressable. High blood pressure, high cholesterol, diabetes, smoking, obesity, and sedentary behavior accelerate plaque buildup and arterial injury, making PAD more likely and more severe.
Common Symptoms of PAD
Do not dismiss leg pain as part of growing old. Seek medical care and screening for PAD if you have these symptoms:
- Claudication: Pain or cramps in the back of your leg while walking or exercising. These pains or cramps go away when walking or exercising stops.
- Rest pain: Burning, aching, or discomfort in the feet or legs while resting—sometimes severe enough to wake you from sleep.
- Skin and temperature changes: Lower legs or feet that are cool to the touch, have shiny skin, decreased or no hair growth, or appear pale when elevated and bluish/purplish when hanging down.
- Weak or absent pulses in the feet or ankles.
- Numbness or tingling in the legs or feet. on-healing wounds or sores on the toes, feet, or legs that do not heal.
Risk Factors You Should Know
Major risk factors for Peripheral Artery Disease include:
- Modifiable: Smoking; high cholesterol; high blood pressure; diabetes; obesity; heart disease.
- Non-modifiable: Age (especially over 65); family history of artery disease.
Addressing the modifiable risk factors—such as quitting smoking, controlling blood pressure and cholesterol, managing blood sugar, maintaining a healthy weight, and staying active—can slow progression or help prevent PAD altogether.
Diagnosing Peripheral Artery Disease
Your Wound Care Center can perform non-invasive tests to diagnose and accurately treat PAD.
Ankle-Brachial Index (ABI)
A simple, painless test that compares blood pressure in your ankle with your arm. A lower ankle pressure suggests narrowed or blocked peripheral arteries and indicates the presence of PAD, though it does not pinpoint exact blockages.
Doppler Ultrasound Test
If the ABI suggests PAD, a Doppler ultrasound uses sound waves to visualize blood flow and identify which artery or arteries are affected. This helps clinicians map blockages and plan treatment.
In some cases, further imaging—like CT angiography or MR angiography—may be used to get a detailed view before considering procedural intervention.
Treatment Options Available for Peripheral Artery Disease
Medical and Interventional Treatments:
- Medications to control cholesterol, blood pressure, and improve circulation (e.g., statins, antiplatelet therapy, cilostazol).
- Supervised exercise therapy: structured walking programs that improve symptoms and blood flow.
- Minimally invasive procedures: angioplasty or stenting to open narrowed arteries.
- Surgical options: bypass surgery to reroute blood flow around severe blockages.
- Wound care: Specialized wound care is critical for PAD patients with ulcers or non-healing sores; it reduces healing time, increases healing success, and markedly lowers amputation risk.
Living with PAD: Lifestyle Changes & Prevention Strategies
Lifestyle modifications that treat and help prevent progression of PAD include:
- Eating a heart-healthy, low-saturated-fat diet.
- Maintaining a healthy weight.
- Engaging in regular, moderate exercise (ideally in a supervised program once diagnosed).
- Quitting smoking.
- Adherence to prescribed medications.
- Routine monitoring of wounds and early intervention for any skin breaks.
Early lifestyle intervention can significantly improve outcomes—small sustained changes have cumulative protective effects on your circulation.
Complications of Untreated Peripheral Artery Disease
- Non-healing ulcers and gangrene.
- Increased risk of severe infection and lower-limb amputation.
- Critical limb ischemia (severe chronic ischemia causing rest pain and tissue loss).
- Elevated risk of systemic atherosclerotic events like heart attack and stroke, since PAD reflects widespread arterial disease.
Early diagnosis and management reduce the likelihood of these serious and potentially limb- or life-threatening outcomes.
When to Seek Medical Help
You should contact a healthcare provider promptly if you experience:
- Leg pain during walking that limits your activity (claudication).
- Rest pain in the feet or toes, especially at night.
- Sores, ulcers, or wounds on your lower extremities that aren’t healing.
- Skin changes (paleness, discoloration, coolness, loss of hair).
- Sudden worsening of symptoms or signs of critical limb ischemia (e.g., severe pain, tissue loss).
If you have multiple risk factors such as diabetes, smoking, or cardiovascular disease, ask about routine screening even before symptoms become pronounced.
The Role of Wound Care in PAD Management
Specialized wound care can reduce healing times, increase healing rates, and significantly lower amputation risks.
PAD reduces the blood flow necessary for normal healing. That makes even minor wounds on the lower extremities dangerous if left unchecked. Wound care teams trained in vascular-compromised healing can:
- Assess wound severity and underlying ischemia
- Apply advanced dressings and therapies
- Coordinate with vascular specialists for optimization of circulation
If you or someone you care for is at risk for PAD and has a wound that is not healing, find a Center near you or request an appointment today.