PAD-Related Ulcers: Causes, Symptoms, and Effective Treatment at Healogics
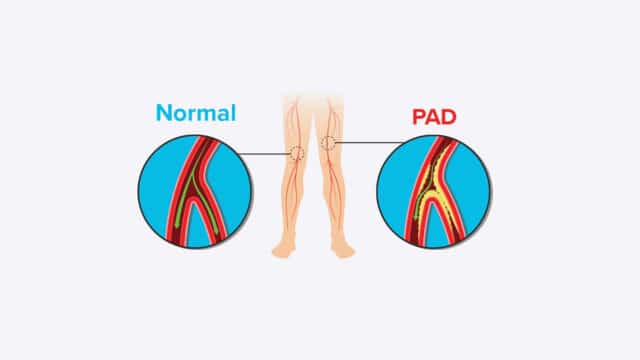
Peripheral artery disease (PAD) is a serious condition that affects millions of people, often leading to significant health issues, including difficult-to-heal wounds. This condition involves the narrowing or blockage of blood vessels in your legs, which reduces blood flow to your feet and lower legs. This decreased blood flow can severely impact the health of your skin and is a common reason why foot ulcers may not heal. Understanding PAD and its connection to wound healing is crucial for effective management and prevention of complications.
PAD and Its Effects on Your Body
What is Peripheral Artery Disease (PAD)?
Peripheral artery disease (PAD) is a condition where the blood vessels in your legs become narrowed or blocked, leading to reduced blood flow to your feet and lower legs. This can significantly affect the health of your skin and is a primary reason why foot ulcers may struggle to heal. It’s estimated that about 8 million people in the USA have PAD, and those with the condition face an increased risk of heart attack and stroke.
How PAD Affects Blood Circulation?
Blood flows through the body in arteries and veins. Arteries carry oxygen-rich blood from your heart and lungs to all tissues, including those in your lower legs and feet, providing them with the vital oxygen they need to stay healthy. Veins, on the other hand, return the used blood to the heart and lungs to be re-oxygenated. When PAD is present, this crucial flow of blood is compromised, leading to a lack of oxygen and nutrients in the affected areas, which can result in PAD skin lesions and other complications.
What causes peripheral artery disease?
Several factors can cause peripheral artery disease. The most common cause is atherosclerosis, often referred to as “hardening of the arteries.” This occurs when arteries become rough and narrow due to the buildup of cholesterol and plaque, effectively blocking the artery. Other causes include aneurysms, damaged or weakened vessels, blood that clots too easily, and abnormal connections between arteries and veins.
Risks for Developing PAD
Certain factors increase your risk of developing PAD. These include smoking, high cholesterol, high blood pressure, diabetes, heart disease, obesity, and a family history of arterial disease. Managing these risks is essential for preventing the onset and progression of PAD.
Learn more detailed information on common risk factors of PAD here.
Common Signs and Symptoms of PAD
Certain factors increase your risk of developing PAD. These include smoking, high cholesterol, high blood pressure, diabetes, heart disease, obesity, and a family history of arterial disease. Managing these risks is essential for preventing the onset and progression of PAD.
Learn more detailed information on common risk factors of PAD here.

Types of PAD-Related Wounds
PAD Ulcers and Sores
Peripheral artery disease can lead to various types of wounds, often referred to as PAD ulcers or PAD sores. These wounds typically occur on the feet and lower legs, especially on the toes, heels, or bony prominences. They are characterized by their punched-out appearance, often with a pale base and minimal bleeding. They can be very painful and are prone to infection due to poor blood flow. It’s crucial to identify these PAD ulcers and wounds early, as they can lead to severe complications if left untreated. The healing process for these wounds is often prolonged due to the underlying circulatory issues.
Treatment and Management Options
Medical Treatments for Arterial Disease
Treating arterial disease, and consequently PAD ulcers, involves a multi-faceted approach. Medical treatments often include medications to dilate vessels and improve blood flow. In some cases, surgical intervention may be necessary to restore adequate circulation. Wound care, as ordered by your provider, is also a critical component of treatment, focusing on keeping the wound clean, moist, and protected to facilitate healing.
Lifestyle Changes for PAD Management
Beyond medical interventions, significant lifestyle changes can greatly aid in managing PAD and preventing future PAD wounds. A diet low in saturated fats and cholesterol is recommended. Moderate exercise, such as walking or biking, can improve circulation. It’s vital to stop or decrease smoking, as it significantly worsens PAD. Losing weight if you are overweight, reducing stress, and avoiding crossing your legs for long periods can also contribute to better health.
Working with your provider to control underlying conditions like diabetes, high blood pressure, high blood cholesterol levels, and managing your weight are crucial steps in preventing the progression of PAD and the development of new ulcers.
When to Seek Professional Help
Warning Signs to Look For
It is important to know when to call your healthcare provider. Seek medical attention if you notice pain or cramps in your calf area while walking or exercising that stops when the activity stops. Other warning signs include pain in your feet or legs while resting, or pain that wakes you from sleep. Lower legs and feet that are often cool to the touch, and legs and feet that appear pale when raised and purplish when hanging down, also warrant a call to your provider. Numbness or tingling in your feet and legs are also indicators that you should seek professional help.
The Role of Wound Care Specialists
Wound care specialists play a vital role in treating PAD ulcers. They can provide advanced wound care strategies, assess the severity of your condition, and work with your provider to develop a comprehensive treatment plan.
Expect a thorough examination, including assessment of blood flow to the affected limb, and a tailored approach to wound management that may include debridement, specialized dressings, and offloading techniques to promote healing.
Prevention and Long-Term Care
Strategies to Prevent PAD Wounds
Preventing new PAD wounds from developing is paramount for individuals with PAD. This involves consistent monitoring of your symptoms and adhering to lifestyle modifications. Maintaining a healthy, low-fat, and low-cholesterol diet, engaging in regular, moderate exercise, and managing your weight are key. It is also crucial to meticulously care for your feet, inspecting them daily for any signs of injury or changes in skin condition. Wearing appropriate shoes that fit well and do not cause pressure points can also prevent sores.
Ongoing Monitoring and Maintenance
Long-term care for PAD involves continuous monitoring and maintenance. Regular follow-ups with your healthcare provider are essential to track the progression of the disease and the effectiveness of your treatment plan. This may include periodic tests to assess blood flow and overall vascular health. Adhering to prescribed medications and continuing with lifestyle adjustments will help to improve blood flow and prevent the recurrence of ulcers.
Your provider can provide instructions and guidance on how to best manage your condition for the long term, ensuring you maintain the best possible quality of life and prevent severe complications like amputation.
If you or someone you care for is at risk for PAD or has a wound that is not healing, find a Center near you or request an appointment today.