Charcot Joint Disease: Symptoms & Treatment

Diabetes affects approximately 9% of the US population—about 30 million Americans—and brings with it a range of potential complications. Among the most serious but lesser-known complications is Charcot foot disease, a condition that can lead to severe deformity, disability, and even amputation if not properly managed.
While Charcot foot is relatively rare, affecting less than 1% of all people with diabetes, its impact can be devastating. Understanding this condition, recognizing its early signs, and seeking prompt treatment can make the difference between maintaining mobility and facing life-altering complications.
Why This Matters: Research shows that diabetic patients with Charcot foot who develop ulcers have a 50% chance of requiring amputation, compared to only 10% for those without ulcers. Early recognition and intervention are crucial for preventing these severe outcomes.
What is Charcot Joint Disease?
Charcot Joint Disease is the abnormal changing of the bones of the feet. The disease was first talked about in the late 1800s by a French physician, Dr. J.M. Charcot. People who had no feeling in their feet were known to have changes in their foot bones. People with diabetes were more likely to have these changes.
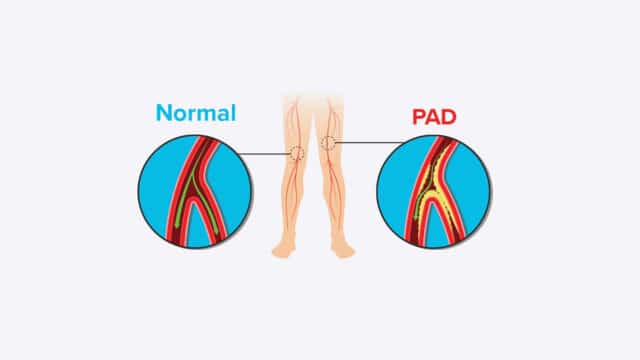
Understanding Charcot Foot Disease: Charcot foot disease (also known as Charcot arthropathy, Charcot neuroarthropathy, or diabetic Charcot foot) is a serious complication of diabetes-related nerve damage (neuropathy) that causes progressive destruction of the bones, joints, and soft tissues in the foot and ankle.
The Medical Definition: This condition occurs when nerve damage prevents you from feeling pain, temperature, or pressure in your feet. Without these protective sensations, injuries that would typically cause pain and prompt you to seek treatment instead go unnoticed. As you continue to walk on an injured foot, the damage worsens, leading to fractures, dislocations, and eventually severe deformity.
What Are the Signs and Symptoms?
- Swelling of the feet
- Increased skin warmth of the feet
- Redness in the involved area
- No sweating in the involved area, leading to dry skin
- Changes in the foot, the foot appears shorter and abnormal
The earliest and most important sign of Charcot foot is often swelling that occurs without an obvious injury. Many patients first notice this when they have difficulty fitting into their regular shoes.
What Are the Risk Factors?
People who are living with diabetes and are unable to feel pain in their feet may develop Charcot Foot. They may have an injury to the foot and not even know it. The person may continue to walk on their feet. This causes further injury that may lead to more injury to the bones and joints.
There may be less muscle strength in the feet and legs when there is no feeling in the feet. This leads to muscle imbalance. That affects how a person walks and can cause more pressure on the bones and joints. This causes even more injury. The person can have twists and sprains without realizing it and continue to walk on their feet.
Primary Risk Factors
Diabetic Neuropathy (Essential Requirement): Charcot foot cannot develop without nerve damage. The loss of protective sensation is the fundamental requirement for this condition to occur.
Obesity (Most Significant Modifiable Risk Factor): Excess weight on a foot that cannot sense pain creates the perfect conditions for Charcot foot to develop. The additional pressure and stress on already vulnerable bones and joints accelerate the destructive process.
Duration of Diabetes: People who have had diabetes for more than seven years are at increased risk, particularly if blood sugar control has been poor during this time.
How Can You Tell if You Have Charcot Foot?
Diagnosis is made by a physical exam, review of the signs and symptoms, and X-ray tests. Diagnosing Charcot foot requires a combination of clinical expertise, imaging studies, and careful evaluation of symptoms. Early diagnosis is crucial for preventing severe complications.
How Do You Treat Charcot Foot?
Prevention of the destruction of the foot is needed. Regular visits to your physician for check-ups, you will need to look at your feet daily, and you may need special footwear. Surgery is sometimes needed. A wheelchair, a cast, crutches, or bed rest may be necessary to help protect your feet.
If the arch of the foot falls, immediate medical attention is needed. Surgery to fuse the bones in the feet may be needed. Treatment may require many months of care to prevent further problems.
Frequently Asked Questions
Can Charcot foot be cured?
While the bone changes from Charcot foot are typically permanent, the condition can be successfully managed. Early treatment can prevent progression and maintain function, but lifelong protective measures are usually required.
How long does treatment take?
The acute phase typically requires 3-6 months of immobilization, followed by 2-3 months of gradual return to activity. However, protective measures and monitoring continue for life.
Will I need surgery?
Not all patients require surgery. Conservative treatment with immobilization and protective footwear is often successful. Surgery is typically reserved for cases with severe deformity or when conservative treatment fails.
Can I prevent Charcot foot if I have diabetes?
Yes, many cases can be prevented through excellent blood sugar control, daily foot inspection, proper footwear, and regular medical care. Early detection of neuropathy is also crucial.
What’s the difference between Charcot foot and a regular fracture?
In Charcot foot, nerve damage prevents you from feeling the pain of fractures, so you continue walking and worsen the injury. Regular fractures cause pain that naturally limits activity and promotes healing.
How do I know if it’s Charcot foot or an infection?
Both can cause swelling, warmth, and redness. However, infections typically involve broken skin or wounds, while early Charcot foot usually has intact skin. The elevation test can help distinguish between them.
Can Charcot foot affect both feet?
Yes, though it more commonly affects one foot at a time. Having Charcot foot in one foot increases the risk of developing it in the other foot.
What happens if I ignore the symptoms?
Ignoring symptoms can lead to severe deformity, ulceration, infection, and potentially amputation. Early treatment significantly improves outcomes and reduces complications.
Expert Care at Healogics
At Healogics, our specialized wound care teams understand the complex challenges of Charcot foot disease. We provide comprehensive care that addresses not only the immediate condition but also the long-term management strategies needed for optimal outcomes.
Take Action Today: If you have diabetes and are concerned about Charcot foot, don’t wait. Early detection and treatment can make the difference between maintaining your mobility and facing serious complications. Contact Healogics today to schedule a comprehensive foot evaluation with one of our wound care specialists.