Granulation Tissue: The Key Indicator of Proper Wound Healing
August 25, 2025
At Healogics, our singular mission is to FIND. TREAT. HEAL.™, so we know the importance of wound healing, which includes healthy granulation tissue. This vibrant, reddish-pink tissue serves as the foundation for wound closure and represents an important milestone in the healing journey. By learning to recognize the signs of healthy versus problematic granulation, we can better guide patients through their treatment process and optimize healing outcomes.
Throughout this guide, we’ll explore the key characteristics of optimal granulation tissue, warning signs that indicate potential complications and effective strategies to promote healthy tissue development. We’ll share our expertise on assessment techniques, intervention strategies, and when to adjust treatment plans based on granulation tissue appearance. Our goal is to equip both clinicians and patients with the knowledge needed to monitor wound progress effectively and ensure the best possible healing environment.
Understanding granulation tissue isn’t just about recognizing its color and texture—it’s about interpreting what these visual cues tell us about the underlying healing process. Join us as we examine this fascinating aspect of wound healing and discover how proper monitoring can transform patient outcomes.
Understanding Granulation Tissue
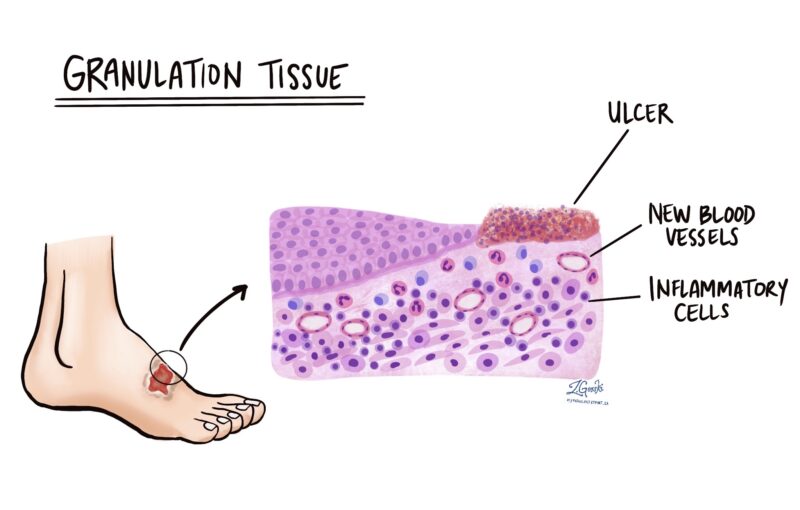
Granulation tissue represents a pivotal phase in the wound healing process—one that bridges the gap between initial injury and final wound closure. Granulation tissue components are the new connective tissue and tiny blood vessels that form on the surfaces of wounds during the healing process. This specialized tissue emerges during the proliferative phase of wound healing and serves as the foundation upon which wound closure and eventual epithelialization will occur.
The composition of healthy granulation tissue is remarkably complex and purposeful. It consists primarily of newly formed blood vessels (capillaries), fibroblasts (cells that produce collagen), inflammatory cells, and a provisional extracellular matrix. This intricate arrangement creates the ideal environment for granulation tissue formation and wound repair, providing both the structural support and nutrient delivery system essential for healing progression.
Healthy granulation tissue exhibits several distinctive characteristics that we train our clinicians to recognize. Optimal granulation appears bright red or pink—reflecting its rich vascular network—and has a moist, granular surface often described as resembling small beads or “berry-like” in texture. Well-formed granulation tissue should be firm but slightly yielding to gentle pressure, uniform in appearance, and evenly distributed across the wound bed. When bleeding occurs during dressing changes, it should be minimal and stop quickly, indicating proper vascular formation without fragility.
We view the development of robust granulation tissue as a critical indicator of healing progression. It not only fills in wound defects and provides the scaffold for re-epithelialization but also supports resistance to infection through increased blood flow and immune cell presence at the wound site. By understanding the normal appearance and function of granulation tissue, we establish a baseline for monitoring wound healing and can more readily identify deviations that might require intervention.
Formation and Development of Granulation Tissue
The formation of granulation tissue is one of the primary pillars of the wound healing process. The process begins approximately 3-5 days after injury, as the wound transitions from the inflammatory phase to the proliferative phase of healing. This transition marks a shift from the body’s initial defensive response to the active, rebuilding process.
The development begins with angiogenesis—the growth of new blood vessels from existing ones. This process is triggered by local tissue hypoxia (low levels of oxygen) and growth factors released during the inflammatory phase, which stimulate granulation tissue formation. When this occurs, endothelial cells from nearby blood vessels begin to migrate into the wound space, forming delicate capillary buds that gradually extend throughout the wound bed. These new vessels create a characteristic red appearance and provide essential oxygen and nutrients to support the healing environment.
At the same time, specialized cells called fibroblasts migrate into the wound, drawn by chemical signals released during inflammation. These cells serve as the primary architects of tissue reconstruction, producing collagen and other components of the extracellular matrix. We typically observe the initial deposition of collagen type III, which later matures into stronger type I collagen as the wound stabilizes.
The developmental timeline follows a relatively predictable pattern when healing progresses normally:
- Days 3-5: Early granulation tissue begins to form with initial capillary budding and fibroblast migration.
- Days 5-7: The tissue becomes more visible, appearing as small, red islands that gradually coalesce.
- Days 7-14: Robust granulation tissue fills the wound defect, assuming its characteristic bright red, granular appearance.
- Days 14-21: Maturation continues with increasing collagen organization and gradual contraction of the wound edges.
Throughout this process, your healthcare team monitors for consistent progression and signs of healthy development. A steady increase in the volume of granulation tissue, uniform distribution across the wound bed, and appropriate color all suggest normal healing advancement. When we observe these patterns consistently, we can help patients understand expectations for their healing timeline and recognize positive signs of progress in their wound healing journey.
Signs of Healthy Granulation Tissue
Healogics considers the assessment of granulation tissue a part of advanced wound care. Recognizing healthy granulation tissue allows us to confirm proper healing progression and identify potential issues before they become significant complications. Through decades of clinical experience and the largest wound database in the world, we’ve identified several key visual indicators that signal optimal wound healing.
Healthy granulation tissue displays a distinctive bright red or pink coloration that is reminiscent of raspberry or salmon flesh and indicates proper vascularization and oxygen perfusion. This vibrant color reflects the dense network of newly formed capillaries that supply the developing tissue with essential nutrients. The color should appear uniform across the wound bed without dark or pale patches that might suggest compromised blood flow.
The texture of well-formed granulation tissue has a characteristic appearance we often describe as “granular” or “beaded.” When examined closely, the surface resembles tightly packed small granules—hence the name “granulation.” This texture should be consistent throughout the wound bed, creating an even surface that gradually fills the wound defect from the base upward. The tissue should appear moist and shiny but not excessively wet or macerated.
Optimal granulation tissue exhibits several additional characteristics that indicate proper healing:
- It should be firm but slightly yielding when gently probed
- The tissue should adhere well to the wound bed without floating or detached areas
- Minimal bleeding should occur when touched during dressing changes
- The tissue should grow at a steady, observable rate, progressively filling the wound space
- There should be no foul odor associated with the developing tissue
We also assess the wound margins, looking for healthy granulation tissue that reaches the wound edges and integrates well with the surrounding skin. This integration creates an optimal environment for epithelial cells to migrate across the wound surface in the final stages of healing.
By regularly monitoring these visual indicators, we can confirm that a wound is following the expected healing trajectory. This assessment guides our treatment decisions and helps us provide patients with accurate feedback about their healing progress. When we observe these positive signs, we can confidently continue current treatment approaches as the wound continues to heal.
Common Issues and Complications
While optimal granulation tissue signals a wound on the path to recovery, we sometimes encounter complications that can threaten the healing process. Identifying these issues early allows us to intervene promptly and adjust our treatment approach before healing stalls or reverses.
Hypergranulation, characterized by excessive growth of granulation tissue that rises above the surrounding skin level, represents one of the most common complications we address. This tissue often appears darker red, spongy, and friable, bleeding easily with minimal contact. We recognize hypergranulation as the body’s response to various factors, including prolonged inflammation, excessive moisture, or friction from dressings. Left untreated, this overgrowth can impede epithelialization and delay final wound closure.
Occasionally, we sometimes observe pale, dusky granulation tissue—a warning sign that indicates inadequate perfusion or oxygenation. This tissue appears light pink, white, or even grayish rather than the vibrant red of healthy tissue. When we note this change, we immediately assess the wound for underlying causes such as pressure on the wound site, vascular insufficiency, or excessive edema. Addressing these underlying factors is often a key part of restoring healthy granulation.
Friable granulation tissue that bleeds easily with minimal contact suggests fragile vascular formation or excessive inflammation. While some minor bleeding during dressing changes is normal, excessive or persistent bleeding indicates abnormal tissue development that may require a modified treatment approach.
Dark, discolored areas within granulation tissue can signal early infection or developing necrosis. We train our clinicians to be particularly alert for brownish, greenish, yellow or black discoloration, especially when accompanied by changes in wound odor or drainage characteristics. These changes frequently occur before more obvious signs of infection and allow for earlier intervention.
Translucent, gelatinous tissue that replaces healthy granulation indicates potential biofilm formation—a challenging complication that requires debridement and antimicrobial strategies. This slick, shiny appearance differs from the granular texture of healthy tissue and can indicate stalled healing and increased bacterial burden.
When we identify these warning signs, we don’t simply note them—we take action. Each complication provides valuable information about underlying issues that may be impeding healing. By recognizing these signals early and implementing appropriate interventions, we can often redirect the healing course and restore the development of healthy granulation tissue, keeping wounds on the path toward complete closure.
The Role of Granulation Tissue in Wound Healing
Granulation tissue is a remarkable biological scaffold that transforms an open wound into a foundation for new tissue development. Understanding its multifaceted role helps us appreciate why promoting healthy granulation is a vital component of our wound management approach.
Granulation tissue serves as nature’s temporary replacement for damaged tissue, filling wound defects and creating a protective barrier against external contamination. This provisional tissue bridges the gap between wound edges and provides the structural foundation upon which final wound closure can occur. We’ve observed that wounds with robust granulation tissue consistently progress toward healing more efficiently than those with poor granulation development.
The rich vascular network within granulation tissue delivers a critical supply of oxygen, nutrients, and immune cells directly to the wound site. This enhanced blood flow supports cellular metabolism and facilitates the removal of waste products and debris. When we assess wounds with healthy granulation, we’re seeing evidence of successful revascularization—a key indicator that the body has established the infrastructure needed for effective healing.
Beyond its structural and vascular functions, granulation tissue actively supports wound contraction. The fibroblasts within this tissue not only produce collagen but also transform into specialized myofibroblasts that generate contractile forces. These forces gradually pull wound edges closer together, reducing the overall wound size and minimizing the area that must be covered by new epithelial cells. We routinely measure wound dimensions to track this contraction process as confirmation of healing progression.
Perhaps most importantly, granulation tissue creates the optimal surface for epithelialization—the final phase of wound closure. As epithelial cells migrate from wound edges across the granulation tissue bed, they require a smooth, moist, and well-vascularized surface. Healthy granulation provides precisely these conditions, allowing epithelial cells to advance in the wound site each day under ideal circumstances.
Healogics also understands that granulation tissue is an active participant in the body’s defense against an infected wound. Its abundant blood supply delivers immune cells directly to the wound site, while newly formed blood vessels facilitate the delivery of systemically administered antibiotics when needed. This defensive capability underscores why wounds with poor granulation are often more susceptible to infectious complications.
By understanding these vital functions, we can better appreciate why promoting healthy granulation tissue formation remains a primary objective in our wound management strategies. When we support optimal granulation development, we’re not simply filling a wound site—we’re establishing the essential foundation for complete wound closure and restoration of skin integrity.
Supporting Healthy Development
Creating the ideal environment for granulation tissue formation requires an approach that addresses both wound-specific and systemic factors. By optimizing these conditions, we can significantly enhance the formation of healthy granulation tissue and accelerate the healing process.
Maintaining appropriate moisture balance stands as perhaps the most critical environmental factor in granulation tissue development. We carefully select wound dressings that create a moist—but not wet—wound site. Too much moisture leads to maceration and potential hypergranulation, while insufficient moisture causes desiccation and impairs cellular migration. Our clinical teams assess each wound’s exudate levels and adjust dressing selections accordingly to maintain this delicate balance.
Proper oxygenation plays an equally vital role in supporting granulation tissue formation. We ensure adequate blood flow to the wound area by minimizing pressure, optimizing positioning, and addressing any underlying vascular issues. For patients with compromised circulation, we sometimes incorporate advanced therapies like hyperbaric oxygen treatment to enhance tissue oxygenation and stimulate angiogenesis—the formation of new blood vessels essential for healthy granulation.
Nutritional support is also important. Granulation tissue components requires substantial protein, vitamins (particularly A, C, and E), zinc, and other micronutrients for optimal development. We regularly assess our patients’ nutritional status and provide targeted supplementation when deficiencies are identified. Even small improvements in nutritional intake can significantly enhance granulation tissue formation.
Temperature regulation also contributes to granulation tissue health. We maintain wound temperature as close to core body temperature as possible, as cellular activity decreases significantly when tissue temperature drops.
Controlling bioburden remains essential for proper granulation tissue formation. We implement appropriate cleansing protocols and antimicrobial strategies to keep bacterial levels below the critical colonization threshold that would impair healing. However, we carefully balance this approach, recognizing that overly aggressive antiseptic use can damage developing granulation tissue.
Finally, we pay careful attention to mechanical factors that impact granulation tissue development. We minimize trauma during dressing changes, select appropriate pressure distribution surfaces, and implement offloading strategies for pressure-related wounds. Additionally, we sometimes employ negative pressure wound therapy to stimulate granulation tissue formation through micro-deformation of the wound bed.
By systematically addressing these factors, we create an environment that optimizes the body’s natural healing capacity. Our approach doesn’t simply manage wounds—it actively promotes the development of healthy granulation tissue that serves as the foundation for complete wound closure and restoration of skin integrity.
Professional Wound Care Management
At Healogics, we view granulation tissue assessment as a core component of our advanced wound care strategy. With over 600 Wound Care Centers® nationwide, millions of wounds treated and our Wound Science Initiative, we’ve developed specialized expertise in monitoring and promoting healthy granulation tissue development—a key indicator of healing progression.
Our approach combines advanced clinical protocols with individualized care plans that address each patient’s unique wound characteristics and underlying conditions. We use assessment tools and measures to monitor granulation tissue quality, allowing for precise tracking of healing progression. This systematic approach helps us identify subtle changes that might indicate potential complications before they become significant barriers to healing.
Professional evaluation of granulation tissue offers distinct advantages. Our wound care specialists are trained to detect nuanced characteristics that might escape untrained observation, such as the difference between healthy granulation and hypergranulation, or early signs of an infected wound that manifest as changes in how the tissue appears. These subtle distinctions often reveal whether a wound will continue healing, stall, or even deteriorate in the healing journey.
Regular professional monitoring also allows for timely intervention when needed. When our clinicians identify concerning changes in granulation tissue, they can immediately adjust treatment protocols, recommend advanced therapies, or address underlying factors affecting tissue development. This responsive approach helps prevent minor issues from developing into significant setbacks.
We understand that wound healing is a complex process influenced by numerous factors. Our integrated approach considers not just the wound itself, but the whole patient, assessing underlying conditions and systemic factors that can impact granulation tissue formation. By combining skilled assessment with comprehensive care, we help guide wounds through the critical phases of healing toward successful closure.
Assessment and Documentation
We employ a structured approach to granulation tissue assessment that combines systematic observation with precise documentation. Our evaluation begins with visual inspection under appropriate lighting, where we assess the tissue’s color, texture, distribution, and relationship to surrounding structures. This visual assessment often reveals subtle cues about healing status that guide our treatment decisions.
During the evaluation, our clinicians document key characteristics using standardized terminology and measurement techniques. We measure the wound bed covered by granulation tissue, noting both quantity and quality. We capture high-resolution photographs with Tissue Analytics, our mobile wound imaging technology, creating a visual timeline that allows for objective comparison of granulation tissue development across visits.
We assess multiple specific parameters during each evaluation:
- Color intensity and uniformity (bright red indicates healthy vascularization)
- Tissue texture and firmness (properly granular vs. friable or mushy)
- Distribution patterns across the wound bed
- Tissue response (slight bleeding vs. excessive fragility)
- Integration with wound edges and surrounding tissue
This information is entered into our electronic health record system, which generates healing trajectory graphs and identifies deviations from expected progress. These tools allow us to quantify healing advancement and recognize stalled progress early, often before it becomes visually apparent.
By maintaining consistent documentation standards across our network, we create comparable data that informs both individual treatment plans and broader clinical protocols. This systematic approach to assessment and documentation ensures that subtle changes in granulation tissue are identified promptly, allowing for timely intervention and optimized healing outcomes.
Treatment Protocols
At Healogics, we implement treatment protocols tailored to the specific characteristics of granulation tissue, along with other factors, that are observed during assessment. Our approach begins with a comprehensive wound evaluation that considers the wound’s history, location, and the patient’s systemic health factors that may impact healing.
Our standard protocols for promoting healthy granulation tissue focus on:
- Maintaining optimal wound moisture balance
- Ensuring adequate perfusion and oxygenation
- Removing non-viable tissue through appropriate debridement
- Managing bacterial balance without damaging fragile granulation
- Controlling edema and inflammation
- Providing appropriate pressure redistribution
We adjust these treatments based on specific tissue appearance:
- Pale or dusky granulation → interventions to improve perfusion and oxygenation
- Hypergranulation → moderate compression or corticosteroid treatments
- Friable tissue → gentler debridement techniques and protective dressings
- Fragmented or patchy granulation → nutritional support and advanced therapies
- Dark or discolored areas → antimicrobial strategies and closer monitoring
Our clinicians follow established Clinical Practice Guidelines based on wound type (diabetic, arterial, venous, pressure injuries, etc.) while personalizing care through our specialized framework for healing. This systematic yet flexible approach allows us to support optimal granulation tissue development while addressing the unique challenges each wound presents.
Promoting Optimal Healing
Healogics implements evidence-based strategies to support healthy granulation tissue formation, recognizing its central role in successful wound closure. Our approach combines clinical expertise with personalized care to create the ideal healing environment.
Maintaining proper moisture balance is fundamental to our practice. We select and apply advanced wound dressings that protect developing granulation tissue while managing exudate and discharge levels, preventing both desiccation and maceration that can impair healing. For wounds with suboptimal granulation, we often employ negative pressure wound therapy (NPWT) to stimulate tissue growth through micro-deformation and controlled fluid removal.
Nutritional support represents another cornerstone of our approach. We assess patients’ nutritional status and recommend appropriate supplementation, particularly focusing on protein, vitamin C, zinc, and other micronutrients essential for collagen production and tissue development.
Minimizing pressure and mechanical trauma protects fragile granulation tissue. We implement offloading strategies for pressure-related wounds and teach proper positioning techniques to prevent disruption of developing tissue. During dressing changes, we employ atraumatic techniques to preserve the integrity of the wound bed.
Regular debridement removes barriers to granulation tissue formation. Our clinicians perform targeted removal of non-viable tissue and biofilm while carefully preserving healthy granulation tissue. This selective approach maintains the wound’s healing momentum while creating space for new tissue growth.
By integrating these strategies into comprehensive treatment plans, we create optimal conditions for granulation tissue development, accelerating healing and improving outcomes for patients with challenging wounds.
Patient Education and Self-Monitoring
We believe informed patients are essential partners in the wound healing process. We educate our patients to recognize signs of healthy granulation tissue—bright pink or red color, moist appearance, and even texture across the wound surface. Understanding these positive indicators helps patients track their healing progress between professional visits.
We also teach patients to identify warning signs that require prompt attention:
- Sudden increase in wound pain or tenderness
- Change in granulation tissue color (darkening, graying, or whitening)
- Increased drainage or change in drainage color/consistency
- Unpleasant odor from the wound
- Redness extending beyond the wound edges
- Fever or general feeling of illness
We instruct patients to contact us immediately if these changes occur, as they often indicate infection or other complications that can rapidly reverse healing progress. Additionally, we emphasize that any significant change in the wound’s appearance or any regression in healing warrants professional assessment.
Through clear education and regular communication, we empower patients to become active participants in their wound care journey while ensuring timely intervention when needed. This partnership approach supports optimal healing outcomes and helps prevent minor complications from becoming serious setbacks.
Advanced Treatment Options
Healogics offers specialized treatments that can accelerate granulation tissue development. Our advanced Wound Care Centers® provide access to cutting-edge therapies not typically available in conventional healthcare settings.
Negative Pressure Wound Therapy (NPWT) remains one of our most effective tools for stimulating granulation tissue formation. This controlled vacuum system creates micro-deformation of the wound bed, increases blood flow, and reduces edema—creating ideal conditions for robust granulation development, particularly in challenging wounds.
Cellular and tissue-based products provide growth factors and structural matrices that jumpstart stalled granulation. These bioengineered tissues introduce essential granulation tissue components that promote angiogenesis and collagen production, especially beneficial in chronic wounds with impaired healing responses.
Hyperbaric Oxygen Therapy significantly increases tissue oxygenation, stimulating the development of new blood vessels and enhancing fibroblast activity. This controlled delivery of 100% oxygen under increased atmospheric pressure creates optimal conditions for granulation tissue formation in hypoxic wounds, those without enough oxygen reaching the affected tissue.
Our debridement techniques precisely remove barriers to granulation while preserving healthy tissue. These approaches create an ideal wound bed that supports rapid development of quality granulation tissue.
By integrating these specialized interventions into personalized treatment plans, we help wounds overcome barriers to healing and establish the healthy granulation tissue essential for complete wound closure.
Working with Wound Care Specialists
FIND. TREAT. HEAL.™ This mission drives our approach to wound care at Healogics, where our specialists bring unparalleled expertise to the assessment and management of granulation tissue development.
Professional wound care offers significant advantages over self-management, particularly when dealing with complex or slow-healing wounds. Our specialists possess the clinical training to detect subtle changes in granulation tissue that often precede more obvious signs of complications. This early detection capability allows for prompt intervention when healing deviates from the expected course.
At Healogics, our wound care experts leverage both advanced diagnostic technologies and clinical experience to evaluate granulation tissue. We can distinguish between healthy development and concerning patterns that might indicate underlying issues such as infection, poor perfusion, or inappropriate moisture levels. This specialized knowledge helps us customize treatment plans to address specific barriers to healing.
Our collaborative approach brings together wound care physicians, specialized nurses, and other healthcare professionals to provide comprehensive care. This multidisciplinary team addresses not just the wound itself, but the full spectrum of factors that influence healing, from nutrition and circulation to glycemic control and mobility.
When patients partner with our wound care specialists, they gain access to evidence-based protocols developed from our experience treating millions of wounds nationwide. Our proprietary clinical pathways guide treatment decisions while allowing for individualization based on each patient’s unique circumstances. This systematic yet personalized approach leads to improved outcomes, reduced healing times, and better quality of life.
By choosing professional wound care management at Healogics, patients benefit from our focused expertise and commitment to healing even the most challenging wounds. Our specialized assessment of granulation tissue represents just one component of our comprehensive approach to wound healing—an approach that has helped countless patients return to health and normal activities.
Ready to Take Control of Your Wound Prevention? Contact Healogics today to schedule your prevention consultation. Together, we can develop a personalized plan to keep you healthy and wound-free for years to come. Click here to find a Wound Care Center® near you.
